View as “PDF version”
Patient Safety Tip of the Week
November 21, 2023
Another
Terrifying MRI Accident
It’s only been a few weeks since we did a column about a
potentially deadly MRI accident (see our October 24, 2023 Patient Safety Tip of
the Week “Serious MRI Accident at
Unregulated MRI Center”). Now an even more terrifying MRI accident
has come to attention.
A nurse was crushed when a hospital bed was pulled into an
MRI machine (Jarosz
2023). The nurse was attending to a patient on a bed at a California
medical center when the bed was pulled by the MRI’s magnetic force, causing the
patient to fall out of the bed and pinning the nurse between the bed and the
MRI machine. The nurse suffered a severe laceration that required surgery,
which included the removal of two embedded screws. She also apparently suffered
injuries to her pelvis, leg and abdomen and spent several days in the hospital
(Mibach
2023). The patient who fell from the bed onto the floor at the time
was not hurt.
The nurse was in the preparation area with a patient and
another nurse. A door between that area and the MRI
room should have been closed but was open. Once the patient was prepped, the
nurse began to move the bed toward the door to the MRI room. However, the door
was open, and as the nurse got closer to the door with the metal bed, she and
the bed were suddenly flung toward the machine,
pinning her between the machine and bed.
KTVU reported the nurse said “I was
getting pushed by the bed” and “Basically, I was running backwards. If I didn't
run, the bed would smash me underneath.” An MRI technologist had just finished
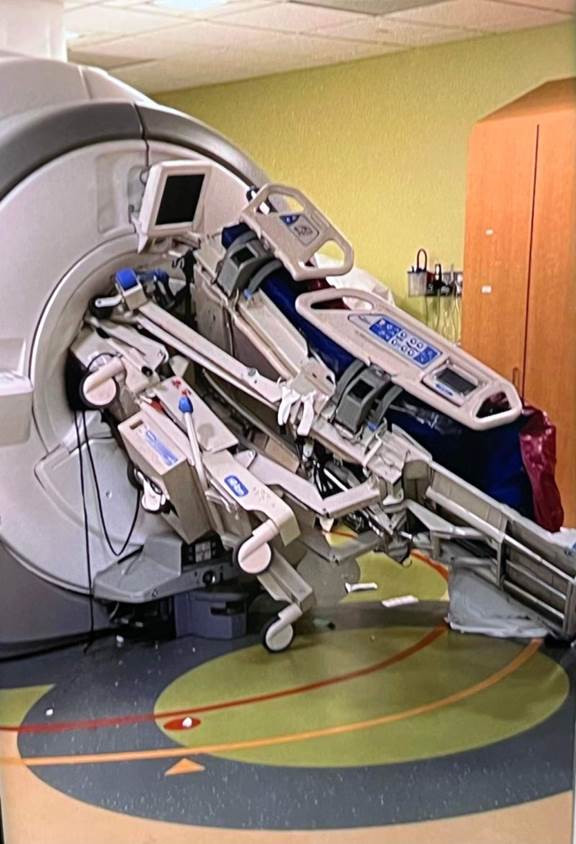
a call and heard screaming coming from another room. The photo below shows the
bed sucked into the MRI machine. It is incredible that someone did not die in
this accident.
A report from the California Division of Occupational Safety
and Health (Cal/OSHA) notes that the nurse and patient care tech were left
unsupervised without MRI personnel. No one, including the patient, was ever
screened. The door to the magnetic room was left open. And the safety alarm
system never sounded. In addition, some employees had not received required safety training and the hospital had failed to
annually test the door alarm as recommended.
This apparently wasn’t the only incident at this hospital. A
photo provided to KTVU shows a medical equipment cart stuck to the MRI scanner,
likely from an incident in March 2015 where no patients or employees were hurt.
The healthcare facility was fined $18,000 by OSHA over the
workplace injury.
Tobias Gilk, arguably the most prominent authority on MRI
safety, has reconstructed the accident from the CMS report (Gilk
2023a) and the OSHA report (Gilk 2023b).
A major contributing factor was the design and layout of the MRI suite. You’ll
want to watch Gilk’s video discussion of that aspect (Gilk 2023b),
in which he demonstrates how the cramped quarters required positioning of
personnel and beds that were critical elements in the accident.
The MRI Imaging
Technician had begun a call to another patient when the bell to Zone III rang. She
asked the MRI Technician if she should answer the door or continue with the
phone call. She was instructed to finish the call and the MRI Technologist
would “get the door”. An RN and a PCT (Patient Care Technician) had arrived
with an ICU patient in an ICU bed. The MR technologist opened the door to Zone
III without first screening the nurse, patient, and PCT in Zone II (Zone II at
this hospital was actually just a hallway used for
general radiology). The required screening of the patient and two non-MRI
personnel was also not performed in Zone III. Intention
was that the patient would be transferred from the ICU bed to a detachable
non-ferromagnetic MR bed/table. It was not clear why that transfer was to take
place in Zone IV rather than Zone III. The MR tech informed the nurse “we are
going in head first” and went back to the control room
to “open the patient chart”. She left the RN, patient, and PCT alone in Zone
III. She said she could not begin the procedure without opening the patient
chart. The control room is out of sight of Zone III. The nurse pulled the ICU
bed into Zone IV (where the scanner is located). The Ferroguard
metal detection system (wall-mounted at the entrance to Zone IV) apparently did
not alarm as the ICU bed was moved into Zone IV. As the bed approached the MR scanner,
the magnetic field powerfully attracted the bed. The patient fell to the floor.
The nurse, who was between the bed and the scanner, was pinned against the scanner.
The MRI Imaging Technician had just finished her phone call when she heard
screaming. She ran into the scanner room and forcibly pulled the nurse from
between the scanner and the bed. The MR technologist did not quench the MR
immediately but had the Clinical Technologist notified to ask if she should do
that. It is not clear how long before the quench took
place.
Key conclusions of the CMS report:
·
The patient, nurse and PCT were not screened in
Zone II prior to entering Zone III
·
The required screening of one patient and two
non-MRI personnel was not performed in Zone III in accordance with the
hospital’s policy
·
The entrance door to Zone IV was left open
·
The hospital did not have a patient interview/clinical
screening area that provided privacy for patients and non-MR personnel that
would facilitate full and complete patient and personnel disclosure of the
medical history. Zone II acts as a buffer between Zone I (general
public area) and the more strictly controlled Zones III and IV. The
facility’s Zone II was located in a hallway used as a
pathway by people entering the Radiology Department leading to other Radiology
services.
·
Neither the MRI Technologist nor the MR Imaging
Technician heard the Ferroguard alarm
·
The Ferroguard alarm
had not been serviced or maintained since purchase and installation in 2014
·
The Ferroguard User
Manual recommends annual testing by manufacturer-approved technicians, daily
qualitative checks, weekly/monthly checks, and what to do if a fault is
suspected. The facility did not comply with those recommendations.
· Director of Imaging said “MRI Technologist felt rushed due to a timed procedure set for 08:00”
·
The hospital did not provide evidence of
MRMS/MRSO annual education or Level II MR safety training.
·
The hospital’s policy and procedures did not
include MRMD and MRSO required MR safety training in their policy
So, what are the lessons learned from this unfortunate but
preventable accident? We see issues in at least the following areas:
·
Training
·
Checking alarms
·
Distractions, interruptions, time pressures
·
Failure to follow protocols
·
Physical layout
·
Quenching
·
Who’s in charge?
·
Failure to learn from prior events?
·
Complacency, normalization of deviance
Certainly, the case illustrates a problem we all deal with –
orienting all staff to MRI safety. That means everyone! It includes not
only newly hired clinical staff, but anyone who might enter the MRI suite at
some time. That could mean your cleaning or maintenance crews. It also means
outsiders like police, firemen, and prison guards who might have need to be at
your MRI unit for one reason or another (see that October 24, 2023 Patient
Safety Tip of the Week “Serious MRI Accident at
Unregulated MRI Center” and our October 21, 2014 Patient Safety Tip of the Week “The
Fire Department and Your Hospital”). And, importantly, it includes temporary staff. Though
the RN in this incident was apparently MR II safety trained (meaning for safety of herself and others), she had been a traveller and had only become employed by the hospital
within the last couple of months. The reports don’t tell us when she had
received that MR safety training. The ACR
Manual on MR Safety definitions of the various levels are listed below.* Was she really trained to that level? And what
about your physicians? How many of you include MR safety training for
your physicians (who might, from time to time, come to the MRI suite). In this
case, even the 2 physicians designated as overseeing MR imaging were said to
have had their MR safety training “during their residencies and fellowships”.
Are they exempt from annual updates? The ACR
Manual on MR Safety says “It is
understood that the MRMD will have the necessary education and experience in MR
safety to qualify as Level 2 MR Personnel. The MRMD, MRSOs, and MRSEs, as well
as all MR Personnel, should undergo MR safety–specific education on an annual
basis.”
A second key lesson is that all your alarm systems need
to be checked regularly. Our February 4, 2014 Patient Safety Tip of the
Week “But What If the Battery Runs
Low?” gave lots of examples of alarms that failed because no one
checked to make sure their batteries were working. But alarms may fail for
other reasons, too. There may be mechanical failures, or someone may have
turned off the alarm purposefully and forgot to turn it back on. In this case, no
ferromagnetic alarm was audible to the MRI technologist or the MR imaging
technician. In this case, the facility was using the Ferroguard
wall-mounted metal detection system. That device shows an amber or red color if
it detects metal and should sound an alarm to prevent entering Zone IV. The Ferroguard User Manual recommends annual testing by manufacturer-approved
technicians, daily qualitative checks, weekly/monthly checks, and what to do if
a fault is suspected. The facility apparently did not comply with those
recommendations. The Ferroguard alarm had not been
serviced or maintained since purchase and installation in 2014. The facility plan of correction notes that Clinical Technology checked
the Ferroguard device at the entrance to Zone IV after
the accident and confirmed “it was functional”. So, the metal detection
capability may have been working but it’s not quite clear whether the alarm was
working or whether the audible level was too low.
In many incidents we see distractions, interruptions,
or time pressures as contributing factors. This case was no different. The
MR Imaging Technician was distracted by the phone call and the “MRI
Technologist felt rushed due to a timed procedure set for 08:00”.
Failure to follow protocols and procedures. The CMS
report showed the following failures:
·
The required screening of one patient and two
non-MRI personnel was not performed in Zone III in accordance with the
hospital’s policy.
·
The patient and non-MRI personnel were left
unsupervised in Zone III.
·
The entrance door to Zone IV was left open.
·
The RN, who was Level II MR safety trained, continued
to move the patient in an ICU bed into Zone IV without stopping for a second screening
in Zone III and transferring the patient to a non-ferromagnetic bed/table.
·
The daily and other periodic checks of the Ferroguard metal detection system were not carried out.
Deficient physical layout. In addition to the physical
layout and design problems noted above by Gilk (Gilk 2023b),
the CMS report notes that Zone II was located in a hallway used as a pathway by
people entering the Radiology Department leading to other Radiology services. The
hospital did not have a patient interview/clinical screening area that provided
privacy for patients and non-MR personnel that would facilitate full and
complete patient and personnel disclosure of the medical history. That is where
initial screening and review of the risk questionnaire would take place.
Like the accident we described in our October 24, 2023 Patient
Safety Tip of the Week “Serious MRI Accident at
Unregulated MRI Center”, there was a delay in quenching the magnet.
Quenching the magnet is a serious event and can give rise to problems of its
own. But both accidents indicate that the staff on-site often feel they do not
have the authority to initiate quenching and those delays in “getting approval”
to quench could have disastrous consequences. It needs to be made clear that a
patient or other person being pinned against the machine is a potentially life-threatening
circumstance that merits immediate quenching.
Who’s running the show? The CMS interviews with the
Chief of Radiology and Imaging Director leave a lot of questions about
oversight of the MRI safety and services. The organization chart had some
handwritten names for key roles. After first stating that the Chief of Radiology
was the MRMD (MR Medical Director), it was later stated that there were 2 MRMD’s,
one from musculoskeletal and one from neurology. A radiologist was identified
as MRSO (MR Safety Officer). But the facility was unable to provide evidence of
MR safety training or credentialling for these roles. Tobias Gilk (Gilk
2023c), in yet another column on this accident, discusses the roles of MRMD
and MRSO in some detail. He notes that the level of MR safety training in residency
and fellowship programs probably does not rise to the level required for an
MRMD. And he notes that the MRSO must be someone who is
readily available in the MR suite, noting that radiologists in a reading room
are probably not appropriate for the role of MRSO. He recommends that certification
should be required for both the MRMD and MRSO roles.
Failure to learn from prior events. You’d be
surprised how often we see an incident occur despite a facility having experienced
a very similar event in the past. We don’t have any details in this case, but
that photo provided to KTVU showing a medical equipment cart stuck to the MRI
scanner, likely from an incident in March 2015, certainly suggests some important
lessons went unlearned.
One can only speculate about the roles
complacency, normalization of deviance, and lack of leadership might have
played as root causes or contributing factors in this accident.
Any facility performing magnetic resonance imaging should be
looking at this accident and the one in our October 24, 2023 Patient Safety Tip
of the Week “Serious MRI Accident at
Unregulated MRI Center”, and asking themselves “Could that actually
happen here?” A thorough review of operations and compliance with policies, protocols,
and procedures is in order and many facilities should consider a full FMEA
(Failure Mode and Effects Analysis).
*ACR Manual on MR Safety Personnel Definitions
Non-MR
Personnel: Patients,
visitors, or facility staff who do not meet the criteria of Level 1 or Level 2
Magnetic Resonance (MR) Personnel will be referred to as Non-MR Personnel.
Level
1 MR Personnel:
Individuals who have successfully passed safety educational efforts as defined
by the facility’s MR Medical Director (MRMD), sufficient to ensure their own
safety and that they do not pose a potential threat to themselves or others as
they work within Zone III will be referred to as Level 1 MR Personnel (eg, MR imaging [MRI] department office staff and patient
aides.) Note that Level I MR Personnel must regularly and routinely work within
Zone III in order for them to maintain their Level 1
status. (For illustration purposes, undergoing a single lecture once a year and
virtually never stepping foot in the MRI suite may be insufficient to satisfy
the requirements of Level 1 MR Personnel.)
Level
2 MR Personnel:
Individuals who have been more extensively trained and educated in the broader
aspects of MR safety issues, including, but not limited to, RF safety,
dB/dt-related safety of time-varying imaging gradients, cryogen safety,
contrast agent safety, etc, will be referred to as
Level 2 MR Personnel (eg, MRI technologists,
radiologists, radiology department nursing staff).
Some of our prior
columns on patient safety issues related to MRI:
·
February 19, 2008 “MRI Safety”
·
March 17, 2009 “More on MRI Safety”
·
October 2008 “Preventing Infection in MRI”
·
March 2009 “Risk of Burns during MRI
Scans from Transdermal Drug Patches”
·
January
25, 2011 “Procedural
Sedation in Children”
·
February
1, 2011 “MRI
Safety Audit”
·
October
25, 2011 “Renewed
Focus on MRI Safety”
·
August
2012 “Newest
MRI Hazard: Ingested Magnets”
·
October
22, 2013 “How
Safe Is Your Radiology Suite?”
·
October
21, 2014 “The
Fire Department and Your Hospital”
·
August
25, 2015 “Checklist
for Intrahospital Transport”
·
August
2016 “Guideline Update for
Pediatric Sedation”
·
October
2016 “MRI Safety: There’s an App
for That!”
·
January
17, 2017 “Pediatric MRI Safety”
·
August
8, 2017 “Sedation for Pediatric MRI
Rising”
·
March
2018 “MRI Death a Reminder of
Dangers”
·
March
2018 “Cardiac Devices Safe During
MRI But Spinners!?”
·
November
2018 “OMG! Not My iPhone!”
·
April 2,
2019 “Unexpected Events During MRI”
·
September
2019 “New MRI Hazard: Magnetic
Eyelashes”
·
October
15, 2019 “Lots More on MRI Safety”
·
November
5, 2019 “A Near-Fatal MRI Incident”
·
November
2019 “ECRI Institute’s Top 10
Health Technology Hazards for 2020”
·
January
7, 2020 “Even More Concerns About MRI
Safety”
·
March
2020 “Airway Emergencies in the
MRI Suite”
·
October
2020 “New Warnings on Implants and
MRI”
·
January
2021 “New MRI Risk: Face Masks”
·
June 1,
2021 “Stronger Magnets, More MRI
Safety Concerns”
·
November
2021 “Yet Another Risk During MRI”
·
January
2022 “MRI Safety Issues”
·
July 26,
2022 “More Risks in the Radiology
Suite”
·
October 24, 2023 “Serious MRI Accident at
Unregulated MRI Center”
References:
Jarosz B. Bay Area nurse crushed in MRI accident
highlighting safety concerns. KTVU 2023; October 27, 2023
https://www.ktvu.com/news/bay-area-nurse-crushed-in-mri-accident-highlighting-safety-concerns
Mibach E. Kaiser Redwood City
fined after MRI machine injures nurse. Daily Post (Palo Alto) 2023; October 20, 2023
https://padailypost.com/2023/10/20/kaiser-redwood-city-fined-after-mri-machine-injures-nurse/
Gilk T. State / Federal Investigation Results from MRI
Accident Available. LinkedIn 2023; August 4, 2023
Gilk T. Video discussing the OSHA report on the MRI
accident.
https://www.tiktok.com/@tobiasgilk/video/7276500408137190702
Gilk T. Who was -organizationally- in charge of MRI safety?
LinkedIn 2023; August 10, 2023
https://www.linkedin.com/pulse/who-organizationally-charge-mri-safety-tobias-gilk-mrso-mrse/
ACR (American College of Radiology). ACR Manual on MR Safety
https://www.acr.org/-/media/ACR/Files/Radiology-Safety/MR-Safety/Manual-on-MR-Safety.pdf
Print “PDF version”
http://www.patientsafetysolutions.com/